One of the greatest challenges we face during the Covid-19 pandemic is dealing with the abnormality of not being able to safely share indoor spaces with people who may, or may not, be infected. Indoor environments carry a particular risk if the SARS-CoV-2 virus that is responsible for Covid-19 is transmitted as aerosols through the air which is trapped for a relatively long time in enclosed spaces.
Covid-19’s Aerosol Threat
On September 10, 2020, Dr Anthony Fauci, director of the NIH National Institute of Allergy and Infectious Diseases, reported in a Harvard Medical School Grand Rounds webcast on the status of Covid-19 transmission that “The aerosol and particle physicists that have approached us now have told us that we really have gotten it wrong over many, many years. Bottom line is, this is much more aerosol than we thought.” He went on to explain that the medical community had been defining the maximum size of an aerosol – a particle small enough to float around in the air for a long time – to be about half that of actual aerosols, including those emitted by a person when they are talking (or just breathing).
For me, this revelation of aerosol classification was not news. What I did find surprising was that medical researchers had been misidentifying the size of aerosols when the physics and methodology for determining the size of aerosol particles and droplets have been in textbooks for decades. In fact, the scientist who essentially defined an aerosol, J.J. Stokes, published his work on the subject in 1851. Physicists are not the only ones who have known this. As a graduate student in mechanical engineering in 1997, I was studying droplet sprays similar to what comes from a cough and spent many hours characterizing how the different sized droplets moved around in a turbulent air stream as they evaporated. Many of the papers I have read on cough sprays were done through university engineering departments, such as this one showing mask effectiveness which was published in June 2020 in the journal Physics of Fluids.
A Multidisciplinary Approach
The effort to figure out how to keep people safe from the Covid-19 virus in public is daunting and multidisciplinary. It requires action from a wide range of top experts in virology, epidemiology, chemistry, fluid mechanics, and other specialized areas. Programs within, or sponsored by, the CDC and NIH are supposed to bring together these knowledge sources to determine all the different mechanisms for transmitting a virus from one person to another through the air, contaminated surfaces, personal contact, or some other means.
Success in the war on Covid-19 is also dependent on the organizational directors, like Dr. Fauci, who oversee these concerted battles, as well as the journalists, politicians, and public safety authorities who provide critical information links between what the experts know and how that knowledge is used to protect the public. If too many of them make uneducated decisions or pass along misinformation resulting from bad assumptions or misinterpretation of research, the value of the work of the experts is greatly diminished. And if those in the most influential roles of government promote disinformation instead of responsibly guiding everyone through the uncertainties of the pandemic, expert analysis and advice have to compete with dangerously absurd speculation.
This is why it is crucial that the experts have a realistic grasp of the limitations of their own research and knowledge when responding to questions. There should be no expectation that any given doctor is also an epidemiologist with insights into how the price of chicken in Thailand may be an indicator of a virus outbreak in Southeast Asia. Likewise, asking an epidemiologist with no clinical experience to diagnose your sinus headache doesn’t make sense. I’m not sure if it is even possible for a single person to have true expertise in every discipline involved in fighting a pandemic, so it is imperative that journalists, government officials, and the public not expect Dr Fauci or any other advisor to necessarily have all the specific answers at hand. Such spokespersons have a responsibility to refer specific questions to individual experts, including engineers and physicists who have been studying the fluid dynamics of sprays for many years. We often want one person that we trust to have all the answers, but that is an unrealistic expectation.
I want to emphasize these points about expertise before diving into a discussion of airborne SARS-CoV-2 transmission that falls into my own knowledge area. Since I have no formal medical training, my explanations of how virus particles travel through the air and some potential remedies must be limited to my education and professional experience in spray behaviour and fluid dynamics. This examination begins at the point when droplets exit someone’s mouth and stop where they land on a surface, get caught in a filter, or are exhausted to the outdoors. It is just one part of the puzzle, but a critical one as Dr Fauci emphasized, that will allow us to figure out the safest way to get people back into public buildings.
Airborne Virus Transmission
You have questions.
The trillion-dollar question of 2020 is how exactly does the SARS-CoV-2 virus jump from one person to another and what is the best way to stop that from happening? Right now, stopping the airborne virus literally means putting up physical barriers, including space, fabric and other sundry filters, plastic sheets, and walls. But with a better understanding of how the virus is transmitted, can we apply a dose of innovation and improve that list of barriers?
What is needed to make classrooms, offices, restaurants, and auditoriums safe for occupancy? For public buildings, guidance usually comes from the American Society of Heating, Refrigeration, and Air-Conditioning Engineers (ASHRAE) and local building and health codes. But are those standards and rules good enough?
Then there are the challenges of actually getting to another building from your home without being exposed to the virus. The number of people who rely on public transportation for at least some portion of their commute is not insignificant and should be taken seriously, especially when it comes to children depending on virus-free busses to get to school. Even if a bus is 100% decontaminated before everyone gets on, will the virus particles from an infected rider get vented out before floating past or landing near other passengers?
We should start looking for answers by first asking one more question: what do we already know about virus transmission through the air and how do we know it?
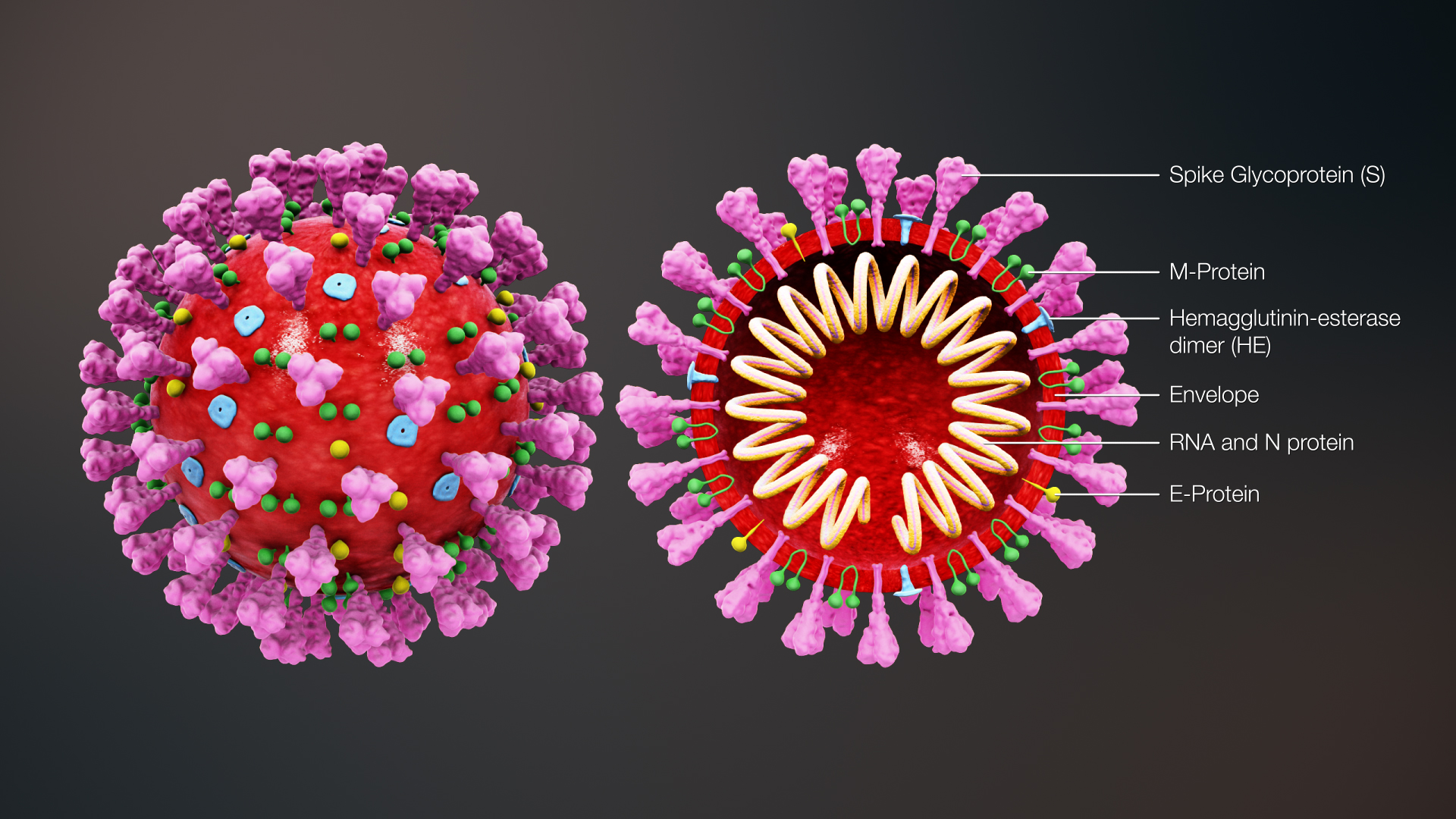
Fortunately, we have the technical ability to look directly at the physical details of an infectious SARS-CoV-2 particle which is a fairly spherical assembly comprised of the virus RNA strands surrounded by a fatty lipid envelope that also incorporates a few different specialized proteins that help with the infection process. When the entire package is intact, it is infectious and called a “virion”. When hunting down virus particles, researchers will mostly come across separated virus RNA or broken envelope proteins, but it is the intact virions that we are concerned about. This species of coronavirus is new and unique, but it is not entirely different from many other viruses, so we can lean on 90 years of virology and fluid mechanics research to get a pretty good picture of how an airborne virion moves from one person to another.
Read more.
Source: Green Roofs.com