NAIROBI, Dec 9 (Reuters) - Africa accounts for 36% of reported cases of the Omicron variant of COVID-19 globally, Richard Mihigo, coordinator of the World Health Organisation's Immunisation and Vaccine Development Programme for Africa, told an online briefing on Thursday.
Source - Reuters
SOUTH Africa’s daily rate of new infections has been on a steady decline for some time. But, truth be told, a fourth wave is probably just on the horizon – and a fifth, and a sixth, and a seventh. This is true of every country in the world.


These waves could be instigated by various phenomena. Perhaps a “super-spreader” event or two, or the arrival of a new and more contagious variant.
Thanks to a successful vaccination programme, smallpox was eradicated worldwide by 1977. But as leading American science journalist Christie Aschwanden recently argued, COVID-19 is unlikely to disappear in the same way. Current vaccines just don’t provide enough protection against infection to provide herd immunity. They provide substantial protection against infection as well as severe illness, but they aren’t bullet proof, and reinfection is a reality.
What does this say about the pandemic?
Epidemics do not require the total eradication of the disease to end. More important than the existence of the disease, is the harm it is causing the population. But will the harms of COVID-19 ever be low enough? Will the epidemic ever end?
In short: Yes, it will – so long as enough people get vaccinated and vaccine efficacy continues to protect people from severe illness with new variants. Although exactly what percentage of the population need to be vaccinated to achieve this is hard to say at this stage.
The pandemic’s end
This won’t happen with a bang. What we can expect to see is a fading-away. Waves might well still continue, and even increase in magnitude. But fatalities will reduce and severe illness become less common as vaccination rates improve.
As medical historians Erica Charters and Kristin Heitman put it, epidemics end once the disease is
accepted into people’s daily lives and routines, becoming endemic— domesticated—and accepted.
Whereas diseases become epidemics and pandemics through purely biostatistical means – a matter of how many people are infected and where those people are – they end once the biomedical harms they cause are sufficiently reduced. In other words, when relatively few people are getting seriously ill.
There are currently multiple vaccines that are extremely effective in reducing the effects of the virus from a life-threatening disease, to (for the vast majority of people) nothing more than a mild cold.
Even in the face of further waves of infection, were the entire population fully vaccinated, the biomedical harm the disease would cause would be (relative to many diseases we are already dealing with) sufficiently low to call an end to the epidemic.
This would mark the point at which governments could stop implementing many of the economically and socially devastating non-pharmaceutical interventions.
How far down the road are we?
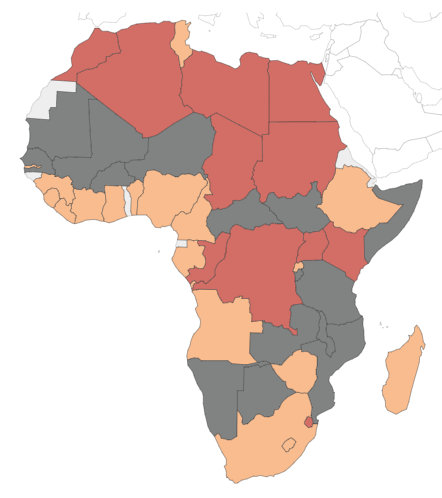
The answer to this question depends on which country you’re living in.
If you are in Europe, you’re closer than those of us living in an African country.
Despite the initial shortages, South Africa currently has more than enough vaccines to satisfy demand. Initially, the slow roll out might have been blamed on supply issues, but now the country faces one big problem: not enough people are choosing to vaccinate.
CONRAD ONYANGO
THE continent’s brightest science students are engaging far more with their African alma-maters, bolstering the quality of academic literature as the COVID-19 pandemic creates new demand for high-end medical research and raising the possibility of a “brain gain” as top students return to the continent.
The Africa Risk-Reward Index 2021, shows the continent is experiencing increased public-private sector funding towards research and development, a trend that could significantly boost African universities’ capacity to retain their best students and increase their competitiveness against global peers.
“The ‘brain drain’ has historically not only weighed on academic output but has also reduced the availability of certain skills. However, this is changing,” says the Index.
Over the last five years, the index shows five African universities have more than doubled the number of published academic papers in numerous fields.
Egypt leads the continent with 4,200 citable academic publications in biochemistry, genetics and molecular sciences published last year- the country is ‘the most prolific producer of this type of research in the continent’.
Most research in the North African country focused on the treatment and prevention of diseases and other medical conditions.
South Africa comes second, with 2,255 publications in 2020, encompassing treatment, prevention, communication, monitoring and diagnosis.
Nigeria (1,290), Ethiopia (501) and Kenya’s (408) might be seen as insignificant but compared to those published five years ago, the increase is remarkable.
In 2015, the number of citable academic publications in the fields of biochemistry, genetics and molecular sciences in Nigeria numbered just 477, Ethiopia 185 and Kenya published just 197.
Tunisia (735) and Morocco (643) in 2020 centred their research work on prevention and diagnosis.
“This trend has been driven by a number of factors including a pick-up in both public and private-sector funding of research and a stronger collaboration between African Alumni and their host universities,” according to the Index.
Analysts at Control Risks and Oxford Economics who prepared the index see Africa continuing to churn out more citable academic papers in future, with the digitalization of education and as scientists collaborate ever-more over the internet to find cures for COVID-19 and other viruses.
The pandemic has increased activities in Africa’s medical sector sparking a series of funding and growth in e-health and biotech as the continent races to manufacture its own vaccines.
In April 2021, Africa Union and Africa Center for Diseases Control and Prevention (CDC) launched Partnerships for African Vaccine Manufacturing (PAVM) that will see African nations build capacity to manufacture 60 percent of vaccines locally by 2040.
In 2020, African markets were a beehive of activity for private sector players seeking to tap into the growing opportunities in biotech and digital healthcare applications.
Investment funding towards African health-tech start-ups grew four-fold in 2020, to 103 million US dollars, defying a pandemic-related slowdown in investment flows to the continent.
Last year, Nigeria launched Africa’s first private lab for human whole-genome sequencing, following a 15 million US dollar fundraise by start-up, 54Gene.
South Africa’s biotech start-up, LifeQ secured 47 million US dollars to meet the rising demand for remote monitoring, while Ghana’s, Yammachi biotechnology received funding from search engine giant, Google to sequence and track COVID-19 variants.
Earlier in the year, Rwanda introduced an investment law to encourage investments in biotech and other technologies in a new Kigali innovation city.
The World Health Organisation has warned that vaccine inequality would affect the Covid-19 fight in Africa and take the world back to square one. Only 3.6% of the continent's population has been vaccinated, while the Covax alliance has cut vaccine shipments to Africa. For more, we are now joined by Dr Mary Stephens the Technical Officer for the World Health Organization Regional Office for Africa.
https://www.youtube.com/watch?v=ovbr46BsG0M