East Africa is in the throes of a public health crisis as its healthcare systems sag under the weight of a rapid third wave of Covid-19, largely blamed on the deadly Delta strain.
But health authorities have identified at least five strains of the coronavirus in the region.
Uganda, which went into lockdown on Friday amid deaths and thousands of new infections, is appealing for help to deal with the crisis in the face of a limping economy, a public healthcare system in a shambles and a population that has been flouting health guidelines set to prevent the spread of the disease.
President Yoweri Museveni announced the cessation of movement across the country for 42 days and a 7pm to 5.30am curfew to help stem the wave of infections which had reached more than 68,000. Forty-two people were reported dead of the virus on Friday, bringing the total death toll to 542.
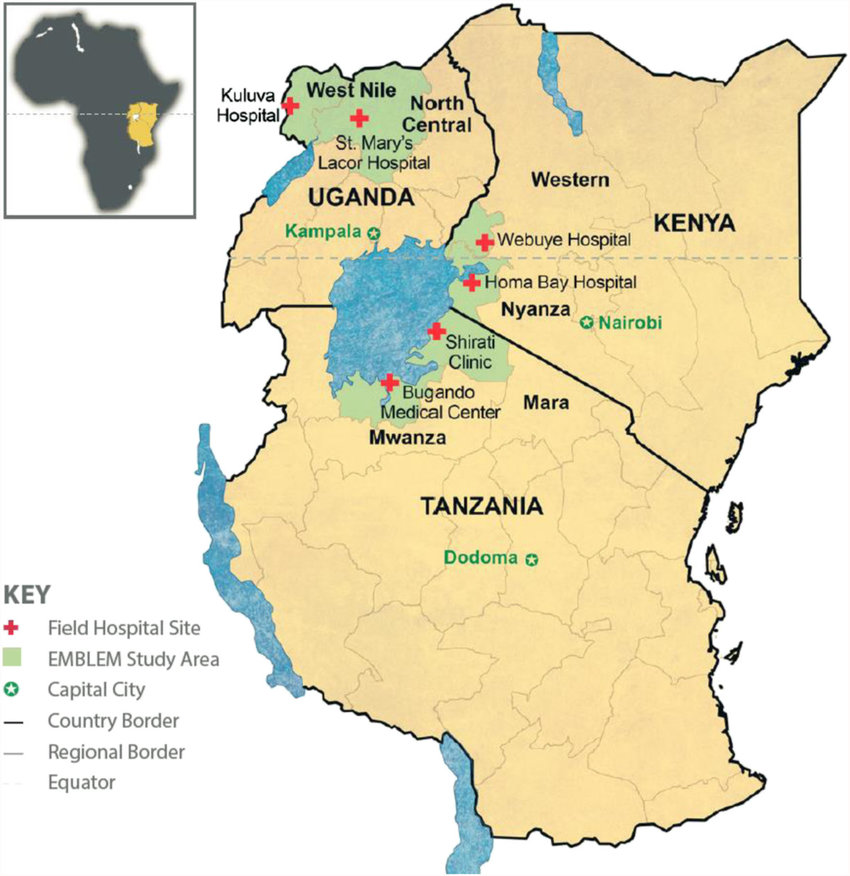
The president announced the new measures to prevent further community transmission as 57 percent of the patients in hospital exhibited severe symptoms. Kampala is leading in infections — 15,347.
The Uganda Virus Research Institute said the Delta strain was brought in by people arriving from India.
In Kenya, it was first reported in Kisumu, and blamed on arrivals from India as well. The first case of the Indian variant was reported in Kenya early May, and Ministry of Health Director General Patrick Amoth said it had been traced back to Indian travellers working in Kisumu.
Kenya has also locked down 13 counties in the west for at least a month, branding them a Covid-19 hotspot.
“There is a risk that the healthcare system in the western region will really get stretched, and if it buckles we are likely to lose many people. The Delta variant is of concern because this variant is more transmissible and probably leads to more serious cases of Covid-19,” Dr Amoth told The EastAfrican in Nairobi.
On Thursday, Dr Monica Musenero Masanza, Uganda’s Senior Presidential Adviser on Epidemics, confirmed that the country had recorded at least five Covid-19 variants.
“We have all the three subtypes of the Indian variant, the South African variant, the UK variant, and Nigerian and Ugandan variants, which are not as virulent as the other three,” she said.
Lack of oxygen and protective gear continues to be a hurdle in the efforts to contain the spread of the disease while cross-border transmission continues due to porous borders and flouting of travel restrictions.
So dire is the situation that on Friday there was speculation that Uganda and Kenya, and even Rwanda – where infection rates have passed seven percent – were contemplating revising the restrictions already in place. Uganda has a curfew in place from 9pm to 5.30am until mid-July and Kenya has announced restrictions starting 7pm to 4am in the counties of Busia, Vihiga, Kisii, Nyamira, Kakamega, Bungoma, Kericho, Bomet, Trans-Nzoia, Kisumu, Siaya, Homa Bay and Migori.
President Museveni, who imposed a partial lockdown after infections hit double digits, has turned to Kenya for help in plugging a gap in the supply of medical oxygen. On Tuesday night, at least 30 patients died at Mulago after the hospital’s oxygen supply malfunctioned. But Mulago’s hospital principal administrator David Nuwamanya on Friday said 17 patients, not 30, “died of severe illness.”
On Thursday, Ugandan Health Minister Dr Jane Ruth Aceng said Kenya had offered oxygen to help avert more deaths.
“We’re having challenges with the availability of oxygen in Uganda for the population that is already infected and those in the isolation facilities. Obviously, with limited oxygen it means we’ll have more deaths,” the minister told a media briefing by the World Health Organisation.
Uganda is also in talks with the Global Fund on acquisition of oxygen cylinders.
“We urgently need 8,000 cylinders of oxygen to cover the entire country, in conjunction with the piped oxygen available in the national and regional referral hospitals,” she said.
“Kenya is in the process of giving us oxygen but then we don’t have the cylinders to fill in the oxygen,” she said as she cautioned that the surging cases in her country should rouse Uganda’s neighbours to take urgent action.
The same day, Kenya declared parts of Western and Rift Valley regions a Covid-19 hotspot.
Health Cabinet Secretary Mutahi Kagwe said the surge in infections in the 13 counties is compounded by their proximity to Uganda.
“There is a heightened risk of cross-border infections from the neighbouring countries, adding to our national caseload,” the minister said.
Uganda has for the past month been experiencing a perilous wave of the coronavirus, which is spiralling out of control.
“The spread has been very aggressive and all the districts have been affected, with the most rampant and heavy transmission majorly in the Capital Kampala and the two districts of Mpigi and Wakiso near the city,” said Dr Aceng.
“The general situation is getting out of hand; there are places where the rate of infection is so high that if you picked any five people, two or more of them would be positive. Covid-19 works by multiplying numbers,” added Dr Musenero.
The sharp rise in cases has meant demand for oxygen by Covid-19 patients has outpaced Ugandan oxygen plants manufacturing capacity.
According to the Daily Monitor, private manufacturers of medical oxygen in Uganda can only produce up to 27.7 million litres of oxygen per day, which is less than half the 62 million litres daily demand in the country.
Alongside other factors, Dr Aceng said, non-adherence to transmission prevention measures has fuelled the new surge that has coincided with the newly imported variants that seem more contagious than the homebred variant.
Covid-19 cases in Africa are surging by over 20 percent week-on-week as the continent’s third wave gains pace and nears the first wave peak of more than 120,000 weekly cases recorded in July 2020, new data from the WHO showed on Thursday.
Uganda is one of the countries with the highest numbers of new weekly cases since the pandemic began. The others are the Democratic Republic of the Congo and Namibia.
As Kampala awaits oxygen from Kenya, ironically, Nairobi is grappling with a similar problem. In Kisumu county, patients are dying because most of the hospitals, more so the ones in the rural areas, do not have the precious commodity.
In neighbouring Homa Bay County, an acute oxygen shortage has been reported. The county has since sought help from Nyamira and Kisumu counties.
All the 32 beds in the High Dependency Unit are full and the number of patients in need of oxygen is increasing.
Dr Peter Ogolla, Homa Bay Referral hospital CEO, said the county is already on the red alert since the hospital has no space.
“What is being strained the most is oxygen supply. If the numbers increase we will be in a crisis, since we are already overwhelmed. Already, eight of our patients are in high flow of pure oxygen,” he said on Friday.
Healthcare workers in public hospitals are referring patients to private oxygen bars where they sell oxygen per hour.
Patients have to wait for days for a free bed before they are placed on oxygen because the wards are full with patients.
The situation is worse in Uganda as it grapples with another wave of the pandemic. Most hospitals, both private and public, report an acute shortage of oxygen so much so that they are no longer admitting patients in the Intensive Care Unit.
Allana Kembabazi, programme manager at the Institute of Social Rights in Uganda, said that Uganda’s oxygen crisis has been in the making for a while, even before the pandemic.
She said that according to the National Scale up for Medical Oxygen Implementation Plan 2018-2022, only four percent of children who died from pneumonia in 2020 received oxygen therapy and only 36 per cent of facilities in the country offering services for chronic respiratory disease had oxygen.
In cases where oxygen is available, a lack of proper maintenance results in frequent non-functionality thus inconsistent supply.
“While it is tempting to blame the insufficient supply of oxygen on the recent surge of cases, oxygen shortage in Uganda has been there for a while now,” she said.
The WHO representative to Uganda Yonas Tegegn Woldemariam said that health authorities are working to address the nationwide shortages.
“We are working with the Ministry of Health to increase oxygen supply including options to import from Kenya,” said Woldemariam.
But, Dr Willis Akhwale, chair Covid-19 taskforce in Kenya, said that while the county is willing to help, the situation at home is critical.
“We don’t have enough. The situation is critical and we are unable to help,” Dr Akhwale told The EastAfrican on Friday.
The Global fund is supporting oxygen supply upgrades in several counties in Kenya, and the Ministry of Health has since ordered some 20,000 oxygen cylinders to support the main supplier, the British Oxygen Company.
“Several oxygen plants that have not been functioning for years are already under repair. Our biggest challenge is piping in most facilities,” he said.
Ironically, Uganda was one of the countries globally lauded last year for its handling of the pandemic, which saw fewer cases and minimal deaths in the months after the lockdown announced by President Yoweri Museveni. Even before the country recorded its first case, authorities announced tough preventive measures, including closing the airspace to passenger planes and all border entry points, banning public transport and non-essential work, closing schools and public gatherings and executing rapid response to alerts within the communities.
Health Minister Dr Aceng became such a popular figure that she decided to run for elective politics a few months later and won a parliamentary seat.
About six months into the pandemic and the country seemed to have contained the spread of the coronavirus, with the number of new cases dropping drastically to a point that no new ones were reported for several days.
Medical workers at the Entebbe Grade B and the Mulago National Referral Hospitals were seen on TV singing and dancing as they saw off the last of their Covid-19 patients.
The country then relaxed restrictions. Many ignored the guidelines earlier put in place.
Ineffective interventions
Now, Uganda has in just a month recorded more than 10,000 infections and at least 150 deaths. Just this week, the country recorded 108 deaths minus those dying from home.
Dr Musenero said that increase in the transmissions indicates that the interventions being undertaken are not effective.
Among the new restrictions is closure of schools, which opened another lid on how the institutions have been hiding cases from parents. Several of these have gone back to communities across the country and are sources of more infections. The government has made it mandatory for teachers to be vaccinated.
The first wave did not affect young people as much but, with the importation of several variants from Nigeria, India, South Africa, United Kingdom and Kenya, the youth are now the biggest risk category.
“Those dying are the young people because they are very many compared to other population groupings. The youth are also the most exposed. We have many of them in hospitals and in home care,” Dr Musenero said.
The increasing numbers have exposed the soft underbelly of Uganda’s health sector. Public hospitals in Kampala and surrounding areas are filled up.
The Entebbe Grade B General hospital and the Mulago National Referral hospitals’ intensive care units are full, according to hospital administrators.
Since the hospitals cannot take in all the numbers in the current wave, Mandela National Stadium has been gazetted as a treatment centre for patients with mild cases but the space there, too, is also filling up.
Health Ministry spokesperson Emmanuel Ainebyona said the ministry is establishing auxiliary treatment centres around the country to accommodate the surging numbers.
“We are also setting up mobile facilities in terms of tents at regional referral hospitals,” Ainebyona said.
Many have opted to go to private hospitals, even when the cost is high, a trend that shows clear distrust of the free government services. Private hospitals require one to pay not less than Ush2 million ($540) before admission and some charge up to Ush5 million ($1,350) a day, an amount too high for ordinary Ugandans.
Those who have visited government hospitals reported a lack of constant medication with claims that they are attended to just once or twice in a day and given mainly painkillers. The Health Ministry said that all patients are attended to with the right medication but more attention is given to the critically ill.
Healthcare workers in the public hospitals are also struggling due to lack of protective gear but Ainebyona said that the ministry is in the process of procuring more gear. At least 2,200 health workers have tested positive for the virus since the pandemic began, with 28 deaths reported.
Uganda’s Covid-19 fight has also been set aback by the unavailability of vaccine doses. The country has been struggling to acquire more doses after a rush for vaccines depleted the 964,000 doses of the AstraZeneca vaccine the country had acquired through the Covax facility.
With India blocking the exportation of more vaccines, Uganda’s vaccination schedule has been altered. This week, the country received 175,000 doses of AstraZeneca, a donation from France through Covax.
According to Ainebyona, these will be administered to people who have already taken the first shot. Uganda is in talks with the US and China to acquire the Johnson and Johnson and the Sinovac doses to speed up vaccinations.
Uganda has also increased vigilance at its entry points and all visitors coming into the country are subjected to a compulsory PCR test while those leaving the country should present negative PCR results.
***
TANZANIA JOINS COVAX
Four months after countries around the world began receiving shipments of free vaccines through Covax, Tanzania is finally joining the initiative, leaving behind Burundi and Eritrea. This reversal in its stance comes in the wake of new leadership in the country, under the presidency of Samia Suluhu Hassan. Upon succeeding John Magufuli, who was one of the continent’s most prominent sceptics about coronavirus. Samia announced the formation of an expert committee to evaluate the nation’s Covid-19 response in early April. The committee recommended that the country join Covax. The country has now submitted its vaccine request form and is currently preparing a vaccination deployment plan, according to the WHO.
- Angela Oketch, Jonathan Kamoga and Pauline Kairu